Skin incisions are commonly treated with photobiomodulation therapy (PBMT) postoperatively to help reduce pain and edema and to decrease healing time.
Intraoperative PBMT is often overlooked, yet research shows it also helps alleviate pain and inflammation, as well as modulate the immune responses and promote tissue regeneration.1
Let’s discuss the use of intraoperative PBMT in general practice.
Intraoperative PBMT
There are several considerations for using intraoperative PBMT instead of postoperative on tissue that has already been closed. The first is the area being treated can be treated much earlier than waiting for the procedure to be finished. One study showed a decrease in inflammation by treating prior to closure, compared to after closure, due to a decrease in the release of cytokines.2
Another consideration is the laser can be directed to the exact area that needs to be treated instead of trying to do it through the closed tissue. The third reason is the beam is less likely to be absorbed by the overlying tissues and red blood cells, allowing for more effective dosing to the targeted tissue.
Asepsis
The fiber cable and handpiece of the laser cannot be sterilized, but it is important to clean those parts in case they are inadvertently exposed to the area being treated. Special care should be taken to remove anything, such as dust or hair, that could fall off the device and onto the surgical field during use.
The veterinary assistant should be gowned and gloved and trained to hold the head of the cable close to area being treated, as well as keeping the cable taut and away from the sterile field (Figure 1). This also requires communication between the surgeon and the person with the laser, as they need to coordinate tissue movement and the equipment. Failure to warn of tissue movement could result in the laser head or cable touching an organ or the sterile field.

Laser settings
The laser setting should not exceed 4W and the target dose can be much lower than what would be used for deep tissue applications: about 3-4 Joules/cm2. Remember tissue has no skin, muscle, or red blood cells through which the beam needs to pass. Normal procedures for external laser therapy involve monitoring the temperature of the skin, but in the operative setting, it obviously cannot be palpated for excessive heat during treatment for deep tissue settings.
It is important to use the same appropriate techniques as you would for a deep tissue treatment. Keep the handpiece moving to allow tissues to thermally relax before returning to the same area.
What can be treated intraoperatively?
Many of the following procedures can be treated both during and after surgery. In the general veterinary practice, some of the more common procedures (i.e. spays, neuters, etc.), should always be considered. Remember, no matter where you are using the laser intraoperatively, it will cause vasodilation, a concern if there is not good hemostasis.
- Ovariohysterectomy. If you are not already doing intraoperative blocks of the ovarian ligaments, consider PBMT after ligation and prior to releasing the ovarian stump. The uterine stump should be treated, as well. Treat the incision postoperatively.
- Orchiectomy. Postoperative swelling is a common issue in many dogs that have been neutered. Treating the stump of the spermatic cord and vas deferens can help mitigate that. The incision and scrotum should be lasered postoperatively, as well.
- Bladder cystotomy. Many dogs and cats experience stranguria secondary to the trauma of a cystotomy incision. As soon as the bladder is closed and prior to returning it to the abdomen, the incision should be treated.
- Hematoma repair. This is a painful and difficult area to block prior to surgery. PBMT can help with pain control.
- Enterotomy/enterectomy/gastrotomy. Healing is always a concern whenever the intestinal or stomach wall is breached. PBMT of the incision and surrounding tissue will lower inflammation and speed healing.
- Orthopedic procedures. Cruciate surgeries (TTA, TPLO, etc.) were among the first procedures to benefit from intraoperative PBMT. Consider using the laser for anything orthopedic, such as fracture repair, patellar stabilization, ununited anconeal, or femoral head osteotomy, to name a few.
- Other considerations. Any other abdominal surgery, such as hemilaminectomy, thoracotomy, ear canal ablation, and urethrostomy.
A few cases
Enterotomy
Foreign body removal is quite common in dogs and cats. Not only is there the insult of the surgery to recover from, but often there is pre-existing trauma that can be quite extensive depending on the type of foreign body, the size of the foreign body, and the time it was in the gastrointestinal tract.
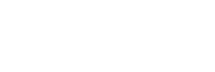
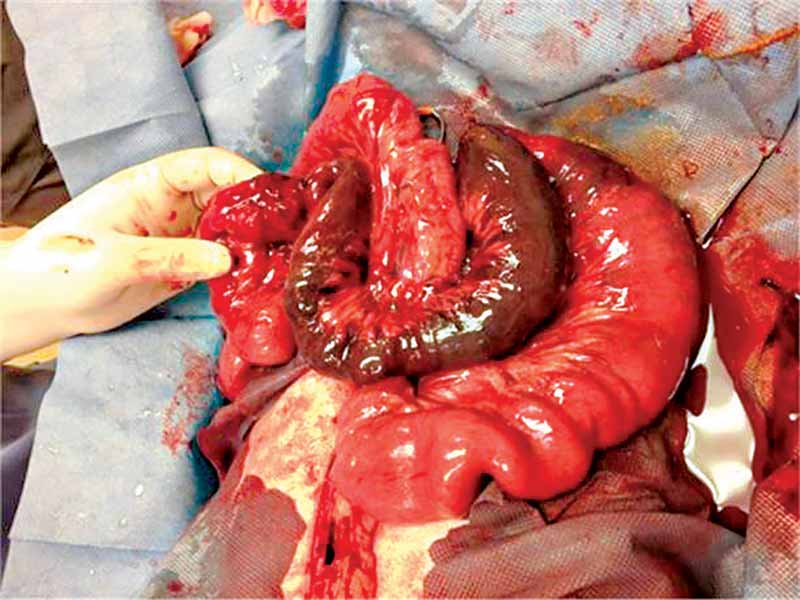
Figure 2 shows the intestinal tract prior to laser treatment and Figure 3 shows the same area immediately after. You can see there is increased blood flow from the color of the intestine, as well as an overall healthier look to it.
Cranial cruciate rupture repair
As in the case of a foreign body mentioned, surgery is already being performed on a traumatized area. There is trauma to the joint structures at the time of the rupture and depending on the length of time prior to surgical intervention, there is going to be varying degrees of damage due to the instability of the joint compounded by the weight of the dog and the degree to which the dog used the injured leg.
We are doing surgery on a leg that already has some degree of insult, and then we add more insultwith whatever procedure we perform. Intraoperative PBMT is indicated and can be done at a slightly higher dose than soft tissue, in the 4-6 joules/cm2 range. Postoperatively, PBMT should be continued on a daily basis for the next week, along with icing, compression and rehabilitation therapy.
Conclusion
PBMT has a known benefit to aid in the recovery of damaged tissue. We often “forget” or “didn’t know” it could be used in the operative setting.
For those of you who have a laser, this is an additional tool for healing and pain control of operative procedures. For those of you who do not own a laser, this is yet another reason to obtain one.
Michael C. Petty, DVM, is a graduate of the veterinary school at Michigan State University. Dr. Petty has devoted his professional life to the care and well-being of animals, especially in the area of pain management. Petty is the past president of the International Veterinary Academy of Pain Management. A frequent speaker and consultant, he has published articles in veterinary journals and serves in an advisory capacity to several pharmaceutical companies on topics of pain management. Petty has been the investigator/veterinarian in 12 FDA pilot and pivotal studies for pain management products. He has lectured both nationally and internationally on pain management topics.
References
- Prior, B. and Millis, D. Therapeutic Laser in Veterinary Medicine. Vet Clin North Am Small Anim Pract. 2015 Jan;45(1):45-56.
- Sakata S, Kunimatsu R, Tsuka Y, Nakatani A, Hiraki T, Gunji H, Hirose N, Yanoshita M, Putranti NAR, Tanimoto K. High-Frequency Near-Infrared Diode Laser Irradiation Attenuates IL-1β-Induced Expression of Inflammatory Cytokines and Matrix Metalloproteinases in Human Primary Chondrocytes. Journal of Clinical Medicine. 2020; 9(3):881.