Malassezia spp. is part of the normal flora of the skin of dogs and cats. When favorable factors occur, such as alterations in skin barrier composition and functions, imbalances in the local microbiome, or an inadequate host immune response, Malassezia can be involved in dermatological diseases, such as seborrheic dermatitis or otitis. Frequently, ear and skin infections occur together.1-3
Otitis complicated with Malassezia (Malassezia otitis or MO) are usually erythematous external otitis with a variable production of yellow or brown waxy-ceruminous secretion.3 Given that Malassezia is highly pro-inflammatory, clinical signs can range from mild or moderate to, rarely, severe and suppurative otitis.3,4
Multiple primary causes of external otitis may favor secondary yeast overgrowth, such as keratinization disorders, endocrine diseases and/or autoimmune diseases, the main one being hypersensitivity diseases. In addition, some conditions predispose a dog to develop MO, such as anatomical anomalies that create ear canal stenosis, increased cerumen secretion, moisture, and reduction of the ear canal ventilation.3
Making a correct diagnosis and management of MO is crucial in veterinary practice, not only to increase our patient’s quality of life, but also because this saprophytic yeast has emerged as an important human pathogen. For example, in neonatal intensive care units, Malassezia systemic infections has been related to infusion of lipid hyperalimentation via deep vein catheters.5
The emergence of yeast resistance against some antifungal drugs in recent years highlights the need for the development of alternative therapies for the control of otitis and dermatitis complicated by Malassezia.

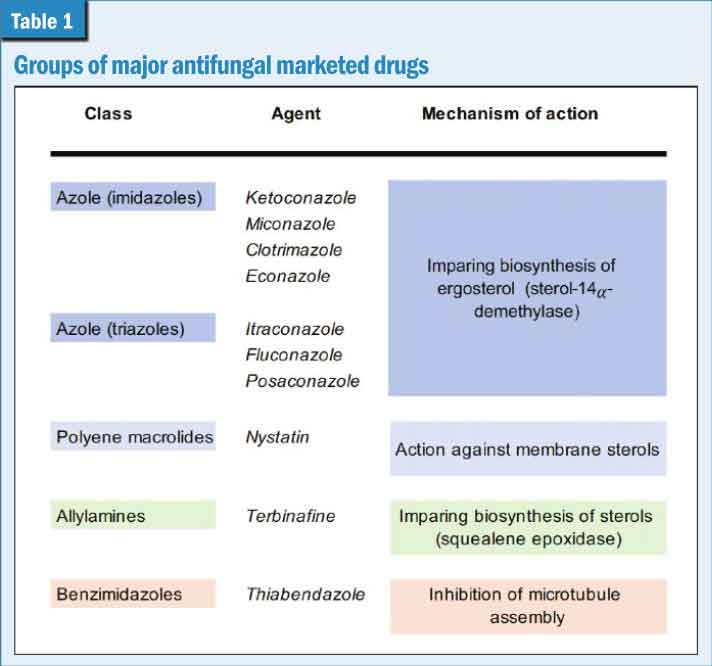
Photos courtesy Isaac Carrasco
Pathogenicity
Malassezia is strongly regulated by the continuous interaction with the host’s immune system, which will determine if there is a progression towards dermatological disease. In addition, coexistence with other microorganisms can affect their pathogenicity and expression of virulence factors.6
An essential first step for colonization is the adhesion of the yeast to the host cells, which is possible by proteins that create a covalent union between the cell wall of the microorganism and the plasmatic membrane of the host’s skin cells. Once adhesion has occurred, yeast proliferates better in environments with a high lipid disposition, since it is a lipid dependent microorganism.
In inflamed and seborrheic skin, there is a high expression of lipases that can damage the skin barrier directly; or by triglycerides hydrolysis, creating an ideal environment for yeast proliferation. Additionally, patients with skin lesions or external otitis produce opioids that increase yeast phospholipase activity.6
When Malassezia proliferates within the stratum corneum, it produces numerous antigens and allergens that can stimulate innate, antibody and cell mediated immune responses, as well as triggering hypersensitivity reactions, giving rise to clinical signs related to dermatitis and otitis.3,6
Incidence of MO
Malassezia otitis is common in dermatological practice. In some studies, Malassezia yeasts were isolated from 72.9 percent of cats and from 57.3 percent of dogs with otitis externa.7 Compared with healthy animals, a higher number of Malassezia yeasts were recovered from animals with otitis, which indicates that such yeasts overgrow in infected sites and play a role in the pathogenesis of otitis externa.8
The yeast population is also influenced by individual and environmental factors. That is why dogs with pendulous ears showed a higher incidence of infection than dogs with erect ears, or the prevalence of positive samples could be higher in winter for cats and in autumn for dogs.8
Diagnosis and management
Cytological study of the aural secretion is the method of choice for diagnosis. There is not a consensus on the minimum number of Malassezia we must observe in an MO cytology. Some authors propose if at least 10 yeast organisms in five fields at 400x magnification are observed in a dog with clinical signs compatible with MO, it should be considered Malassezia is implicated in otitis.6,8
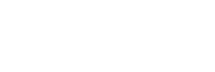
Some groups of drugs can be effectively used for controlling MO, with different mechanisms of action and pharmacokinetics/pharmacodynamics characteristics (Table 1).
Azoles are the most commonly used antifungal drugs; among them, ketoconazole and itraconazole present the lower minimum inhibitory concentrations (MIC) for Malassezia in some studies.9-11
Regardless of the drug chosen, the topical route is the ideal one for the treatment of MO. Using systemic antifungal medications for controlling MO is often associated with poor efficacy owing to inadequate drug penetration into the ear canal lumen.12
Drug resistances
Knowing in detail the incidence of pharmacological resistance to antifungals by Malassezia is not easy, perhaps because they are underdiagnosed or perhaps due to the technical difficulty that exists in many countries to carry out a correct anti-fungi gram and to know the MICs.3 Despite this, multiple mechanisms by which yeasts can become resistant to antifungals have been studied. For example, since azoles inhibit the function of lanosterol 14-a-demethylase (fundamental for producing ergosterol), Malassezia have developed mutations in the gene that codes for the ERG11 enzyme.11
When we talk about microbiological resistance, we mean, based on the results obtained in vitro, the microorganism can only be controlled using doses exceeding the therapeutic safety margin for the patient. These results obtained in vitro will not always perfectly predict the behavior of the drug in vivo, which can be influenced by clinical and pharmacodynamic factors.1,3
For example, for topical antifungals, which is the optimal therapeutic route for treating MO, resistance based on increased MIC values would be indeed poorly significant from a clinical perspective, since topical medications may have a 1,000-fold higher concentration.3
Still, in dogs with chronic otitis, compared to dogs with acute otitis that had not previously received antifungals, yeasts with a significantly higher MIC have been isolated for some antifungal drugs. These findings may indicate the possibility of resistance developing during treatment, even a topical treatment.13,14 Likewise, some studies show that dogs with dermatitis present Malassezia populations with a higher resistance profile.15
Further, it has been observed that many Malassezia strains are large producers of biofilm (up to 83 percent of the strains are capable of producing biofilm, with variable intensity).9,16 That plays an important role in antifungal resistance.16 It has been observed that higher concentrations of drugs will be necessary for their treatment, since in some studies, between 83 and 100 percent of microorganisms embedded in biofilm were resistant to the commonly used concentrations of drugs with which they were treated.
In fact, some biofilm embedded Malassezia presents MICs 2,000 times higher than in the planktonic form.5 That is why it is essential to recognize and treat biofilm to avoid underdosage and the development of further drug resistances.
Antifungal alternatives
Ear cleaning is a common practice to help treat otitis externa and to prevent recurrence in dogs prone to otitis. There is a wide range of cleaning products with a variety of active ingredients, some of them with antimicrobial activity that limits the proliferation of bacteria and yeast, helping to prevent recurrent infections.17-21 Most cleaning products contain organic acids, such as boric acid and glycolic acid. Boric acid exhibits astringent capacity, helps buffer the ear canal environment, and has a mild acidifying action. An ear canal pH greater than 6 is associated with infection in dogs, and pH-modifying ear cleaners can inhibit microbial growth.22
Boric acid is commonly used as a treatment for human fungal otitis and has anti-Malassezia activity used at two percent concentration.23 Glycolic acid, an alpha-hydroxy acid, improves epidermal renewal and desquamation, stabilizing the ear canal microenvironment and thereby preventing the proliferation of microorganisms.
In view of the actual global problem of bacterial resistance, it is worth pointing out that ear cleaners with activity against Malassezia may help to reduce the unnecessary use of antibiotic-containing polypharmaceutical ear medications.21
As mentioned, MO used to be secondary to primary underlying disease or predisposing factors, allergic dermatitis being the most common. To achieve therapeutic success, it is mandatory to control the allergic-related inflammation. Topical corticosteroids are commonly used in a pulse basis, that sometimes are added to the otic cleaners, to decrease the incidence between otitis externa flares in allergic patients, keeping the ear microenvironment stable24 without affecting the stability of the normal ear microbiome.25
Conclusion
The use of antifungal drugs can be useful for rapid control of yeast overgrowth, although recurrences are frequent, generally due to poor management of the underlying cause of the MO (mainly allergic dermatitis). Such indiscriminate use of antifungal drugs may lead to the emergence of drug resistances by Malassezia and limit the therapeutic success.
In addition, since most of the antifungals marketed for treatment of MO are accompanied by antibiotics, they must be avoided, when possible, to use both groups of drugs responsibly. This is to help reduce antibiotic drug resistances seen in the last few years, both in veterinary and human medicine.
Antiseptics are widely used to control ear and skin bacterial and yeast infections. Ear cleaners with activity against Malassezia help to reduce the unnecessary use of antifungal and antibiotic drugs, especially the polypharmaceutical ear medications.
Isaac Carrasco, DVM, PhD, is a graduate of Universitat Autònoma de Barcelona in Spain. Dr. Carrasco is accredited in Dermatology by AVEPA and GPCertDerm. Carrasco is the head of dermatology service at Anicura-Glòries (Barcelona, Spain) and Evidensia-Canis Mallorca (Palma, Spain) Veterinary Hospitals, and has authored numerous national and international publications.
References
- Gaitanis G, Magiatis, P, Hantschke, M, et al. The Malassezia genus in skin and systemic diseases. Clin Microbiol Rev 2012; 25, 106–141. https://pubmed.ncbi.nlm.nih.gov/22232373/
- Niae S, Yurayart C, Thengchaisri N, et al. Prevalence and in vitro antifungal susceptibility of commensal yeasts in the external ear canal of cats. BMC Vet Res 2021;17(1):288. https://bmcvetres.biomedcentral.com/articles/10.1186/s12917-021-02995-7
- Peano A, Johnson E, Chiavassa E, et al. Antifungal Resistance Regarding Malassezia pachydermatis: Where Are We Now? J Fungi (Basel) 2020;6(2):93. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7345795/
- Nunes-Rodrigues TC, Vandenabeele SI. Pilot study of dogs with suppurative and non-suppurative Malassezia otitis: A case series. BMC Vet Res 2021;17(1):353. https://bmcvetres.biomedcentral.com/articles/10.1186/s12917-021-03066-7
- Figuereido LA, Cafarchia C, Otranto D. Antifungal susceptibility of Malassezia pachydermatis biofilm. Med Mycol 2013;51(8):863-7. https://pubmed.ncbi.nlm.nih.gov/23834283/
- Bond R, Morris DO, Guillot J, et al. Biology, diagnosis and treatment of Malassezia dermatitis in dogs and cats Clinical Consensus Guidelines of the World Association for Veterinary Dermatology. Vet Dermatol 2020;31(1):28-74. https://pubmed.ncbi.nlm.nih.gov/31957203/
- Cafarchia C, Gallo S, Capelli G, et al. Occurrence and population size of Malassezia spp. in the external ear canal of dogs and cats both healthy and with otitis. Mycopathologia 2005;160(2):143-9. https://pubmed.ncbi.nlm.nih.gov/12058723
- Cafarchia, C, Gallo S, Capelli, G, et al. Occurrence and population size of Malassezia spp. in the external ear canal of dogs and cats both healthy and with otitis. Mycopathologia 2005, 160, 143–149. https://pubmed.ncbi.nlm.nih.gov/12058723
- Nogueira-Brilhante RS, Gleiciane da Rocha M, De Melo-Guedes GM, et al. Malassezia pachydermatis from animals: Planktonic and biofilm antifungal susceptibility and its virulence arsenal. Vet Microbiol 2018 Jul; 220:47-52. https://pubmed.ncbi.nlm.nih.gov/29885800/
- Yurayart C, Nuchnoul N, Moolkum P, et al. Antifungal agent susceptibilities and interpretation of Malassezia pachydermatis and Candida parapsilosis isolated from dogs with and without seborrheic dermatitis skin. Med Mycol 2013;51(7):721-30. https://pubmed.ncbi.nlm.nih.gov/23547880/
- Kano R, Aramaki C, Murayama N, et al. High multi-azole-resistant Malassezia pachydermatis clinical isolates from canine Malassezia dermatitis. Med Mycol 2020;58(2):197-200. https://pubmed.ncbi.nlm.nih.gov/31329927/
- Morris DO. Medical therapy of otitis externa and otitis media. Vet Clin North Am Small Anim Pract 2004; 34: 541–555. https://pubmed.ncbi.nlm.nih.gov/15062623/
- Chiavassa, E, Tizzani P, Peano A. In vitro antifungal susceptibility of Malassezia pachydermatis strains isolated from dogs with chronic and acute otitis externa. Mycopathologia 2014, 178, 315–319. https://pubmed.ncbi.nlm.nih.gov/25031085/
- Kano R, Kamata H. Miconazole-tolerant strains of Malassezia pachydermatis generated by culture in medium containing miconazole. Vet Dermatol 2020;31(2):97-101. https://pubmed.ncbi.nlm.nih.gov/31729813/
- Cafarchia C, Figueredo LA, Iatta R, et al. In vitro antifungal susceptibility of Malassezia pachydermatis from dogs with and without skin lesions. Vet Microbiol 2012;155(2-4):395-8. https://pubmed.ncbi.nlm.nih.gov/21962411/
- Conkova E, Proskovcova M, Vaczi P, et al. Vitro Biofilm Formation by Malassezia pachydermatis Isolates and Its Susceptibility to Azole Antifungals. J Fungi (Basel) 2022;8(11):1209. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9693420
- Mendelsohn CL, Griffin CE, Rosenkrantz WS, et al. Efficacy of boric-complexed zinc and acetic-complexed zinc otic preparations for canine yeast otitis externa. J Am Anim Hosp Assoc 2005;41(1):12-21 https://pubmed.ncbi.nlm.nih.gov/15634862/
- Bensen CE. Susceptibility of selected otitis externa pathogens to individual and mixtures of acetic and boric acids. Proc Annu Am Acad Vet Derm/Am Coll Vet Derm 1998; 14:121.
- Nenoff P, Haustein U-F. In vitro activity of phytosphingosines against Malassezia furfur and Candida albicans. Acta Derm Venereol 2002;82(3):170-3. https://pubmed.ncbi.nlm.nih.gov/12353705/
- Puigdemont A, d’Andreano Sa, Ramió-Lluch L, et al. Effect of an anti-inflammatory pomegranate otic treatment on the clinical evolution and microbiota profile of dogs with otitis externa. Vet Dermatol 2021;32(2):158-e37. https://pubmed.ncbi.nlm.nih.gov/33399257/
- Mason CL, Steen SI, Paterson S, et al. Study to assess in vitro antimicrobial activity of nine ear cleaners against 50 Malassezia pachydermatis isolates. Vet Dermatol 2013;24(3):362-6, e80-1 https://pubmed.ncbi.nlm.nih.gov/23551137
- Swinney A, Fazakerley J, McEwan N, et al. Comparative in vitro antimicrobial efficacy of commercial ear cleaners. Vet Dermatol 2008;19(6):373-9. https://pubmed.ncbi.nlm.nih.gov/19055612/
- Bassett RJ, Burton GG, Robson DC et al. Efficacy of an acetic acid/boric acid ear cleaning solution for treatment and prophylaxis of Malassezia sp. otitis externa. Aust Vet Pract 2004; 34: 79–82. https://www.researchgate.net/publication/287872287
- Bergvall KE, Ahman S, Mueller R, et al. Can topical hydrocortisone aceponate effectively control allergic otitis externa and reduce the risk of recurrence? A double blinded, placebo-controlled, prospective study. Vet Dermatol 2017; 28: 535.
- Leonard C, Timiniau B, Ngo J, et al. Preventive use of a topical anti-inflammatory glucocorticoid in atopic dogs without clinical sign of otitis does not affect ear canal microbiota and mycobiota. Vet Dermatol 2021;32(4):355-e98. https://pubmed.ncbi.nlm.nih.gov/34033155/