Photos courtesy Michelle Evason
In dogs, hot spots are one of the most common skin disease presentations to veterinary clinics and ERs, particularly over the summer months. These painful, sticky, and itchy-scratchy, swollen lesions are dog-self-induced in reaction to something that hurts, itches, or both. Underlying causes range from parasites (e.g. fleas), painful joints, to skin barrier damage (e.g. grooming incident or ears/otitis), and include underlying adverse reaction to food, and atopy.1
The cycle of inflammation usually kicks into high gear (and this can occur uber-quickly) after the dog’s own colonizing bacteria (frequently Staphylococcus pseudintermedius) shift to infection at the damaged site.1
In clinical practice, canine hot spots bring other considerations besides dog (and pet owner) discomfort and need for relief. One of these is appropriate antimicrobial use, as antimicrobial resistance (AMR) is rising, and dermatologic concerns are one of the most common reasons for veterinary antibiotic use.2,3 Another consideration may be veterinary management and care costs, as it is a time when clients may say, “We’re limited in what we can spend.”
Pet owner budget and needs are key components in effective delivery of veterinary care, and incorporation of spectrum of care, defined as evidence-based veterinary medicine (EBVM) options along the socioeconomic spectrum, can be helpful for vets, pets, and pet owners.4 Examples of EBVM decision-making for pet health issues (parvo, heartworm) have been provided in past articles, along the spectrum of care, and effective treatment of hot spots is another common presentation for general practitioners.
Clinical ‘hot spot’ case
You probably remember late-night (or morning or afternoon) cases like Jimmy Chew’s (JC): The poor little fellow, a six-year-old, male, neutered, mixed-breed dog, was incessantly licking, biting, itching, scratching, and tearing at a spot on his skin. JC’s owner brought him in to the ER to see me because he could not sleep (work, or anything else), as JC could not either.
JC presented for “0 to 60” itching, which started that day. His vaccines were up to date, he was eating a commercial diet well, did not have a history of skin concerns, and his physical exam was clinically unremarkable, aside from a hot spot on his body, measuring 8 cm x 5 cm. It was red, raw, and had papules, pustules, and crusts; it looked like a classic angry and painful pyoderma.
EBVM and spectrum of care
Let’s implement EBVM and spectrum of care for JC and his people, something I sincerely wish I could have done during my ER days. Utilizing our prior spectrum of care tactics and asking a targeted clinical question about JC’s hot spot concern can provide a framework for addressing key aspects of his visit to the clinic.4-7
Step 1: Defining the clinical question.
Question development is critical for a speedy literature search. In JC’s case, the question could be around treatment for hot spots (i.e. topical vs. systemic/oral antibiotics) and our (and JC’s) major outcomes of interest: Stop the itch/pain (reduce illness), fix it, and ideally stop it from happening again (resolution/ prevention), along with being mindful of costs and appropriate antimicrobial use/stewardship.
Here, our Patient/Population-Intervention-Control/Compare-Outcome (PICO) clinical question might be: “In dogs, like JC, with a hot spot (P), does topical therapy (I), as compared with oral antimicrobials (C), alter chance of resolution (O)? What’s the evidence?”
Step 2: Summarizing the scientific evidence (Table 1). Create a summary of a brief (10 to 15 minutes) veterinary literature search and critical appraisal using the PICO question and a freely available online search engine (i.e. PubMed.gov).
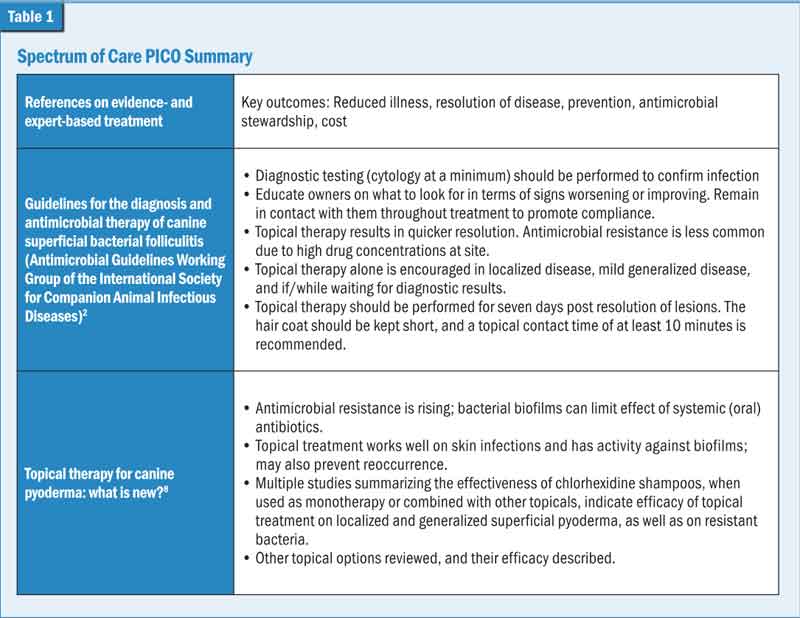
Step 3: Reviewing the evidence
JC’s owners were advised, based on EBVM assessment, that topical therapy is equivalent (and preferable) to systemic (oral) antimicrobials in uncomplicated cases like his. Cytology of the lesion/pustule would be optimal for diagnosis, and would help identify bacterial presence and type (i.e. cocci, rods), determine co-infection (e.g. Malassezia), and aid treatment recommendations.
However, if cost is a concern, shared decision-making on cytology can happen. For example, further discussion with JC’s owner, in addition to the above, might include reviewing why cytology information is helpful, particularly if the hot spot does not look like the usual type, (e.g. no pustules); or that culture and susceptibility (C/S) testing would be sensible if JC had been treated with oral antibiotics in the past and did not respond as expected. Communicating there are other differentials for hot spots, such as ringworm (dermatophytosis) and demodicosis, which may not respond the same way, will also be important. Further, and as with all client conversations, remember to include this information in JC’s medical record.
Other factors and shared decision-making that may impact treatment recommendations, in addition to antimicrobial stewardship and cost, would include the extent and severity of JC’s skin lesions, his haircoat, temperament (i.e. Is topical treatment an option?), and do-ability (Can the owner commit to care?), along with signs of a concurrent disease process. From a testing standpoint, bacterial C/S would be advised if systemic (oral) antimicrobial drugs had been used and we are concerned about methicillin-resistant Staphylococcus pseudintermedius (MRSP). With topical therapy, another advantage is that bacterial type (or whether MRSP) really does not impact therapy/management, and as such C/S is not typically indicated.
After taking all this into account and reviewing the EBVM findings, topical over-the-counter (OTC) therapy (without oral antimicrobials) is the advised approach for JC’s hot spot, unless this is precluded by dog or pet owner reasons.
Topical treatment is advised as the lesion is localized, in the early stages (milder), and as it appears that JC’s underlying reason for dog-induced trauma may be a lack of preventive care for ectoparasites (i.e. fleas, as noted on his physical exam). Other therapies to help JC include anti-inflammatories (e.g. short course of steroid or topical) to alleviate discomfort and relieve the immediate need to itch, scratch, and bite.
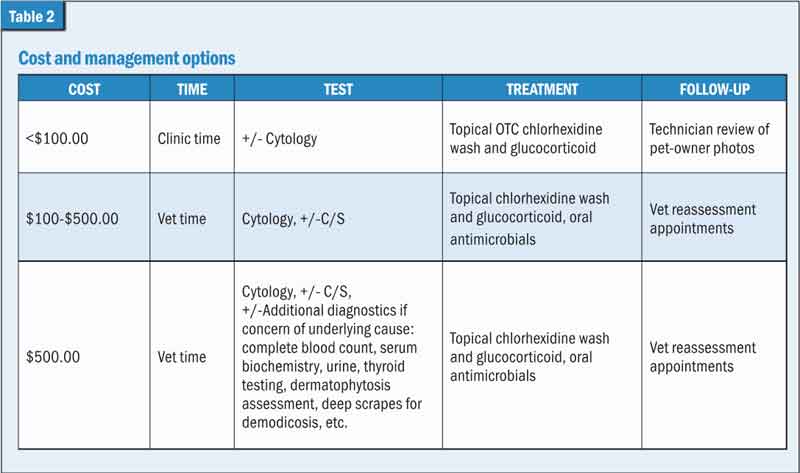
Step 4: Communicating cost and management options (Table 2)
Fee estimates will vary based on regional guidelines. As a rough example of cost, your consultation/exam fee and cytology (cocci noted) may already be at about $70-$100. This may also include palliation to ease patient discomfort and, after cytology has been collected, clipping of the hair, topical cleaning, and glucocorticoids.
Step 5: Shared decision-making outcome
JC did great with our spectrum of care. In his case, the lowest cost option was selected, and cytology (cocci) was performed by a visiting veterinary student at the clinic. Topical antimicrobials (chlorhexidine wash) and a steroid cream were prescribed, and technician photo image review were coordinated with the pet owners to check in on how things were going.
Additionally, spectrum of care plans for the longer term were discussed, made, and budgeted for to help prevent further reoccurrence/flare-ups and provide other age- and region-appropriate preventive care (e.g endo-parasites). By day two, JC’s hot spot pictures were drastically improved; and by day seven, his hot spot was only a “K9 memory.” As a side note, ideally, parasite prevention would be discussed, and begun (based on risk, region), at the first puppy exam. Flea infestation is another infectious disease entirely preventable with regular and consistent veterinary product compliance.
Limitations of EBVM
As is frequently the case, further studies are needed to develop and fine-tune protocols for topical therapy (i.e. frequency of application, duration of treatment, contact time of agents). In general, focal lesions may do best with ointments that provide a longer contact time for bacteria, while more widespread lesions might be best tackled with chlorhexidine shampoos. Further, decreasing the amount of time/effort owners need to nurse their pets will directly increase veterinary compliance. An example of this might be the use of a spray instead of a shampoo.
Spectrum of care can help with delivering day-to-day veterinary care, particularly with “cost-limited” conversations, and may help ease its burden on veterinary team members. Providing education on outcome- and option-based management and preventive care in an individualized and shared decision-making way can be useful for dogs like Jimmy “no-longer-Chews” and hopefully learning about his case will assist in your day-to-day with other patients.
We are truly lucky in this profession to have the skillset, creativity, and compassion in assisting our clients and their pets across a spectrum of care needs.
|
INCORPORATING EBVM IN COST OPTIONS |
| Below are examples of client communications for these cost ranges.
Spectrum of care for $100. Provided this is a typical uncomplicated hot spot, treatment with chlorhexidine wash and glucocorticoid should resolve JC’s signs. Ideally cytology is performed to confirm the presence of bacteria and determine whether typical for Staph spp. or if other fungi, parasites, or bacteria are involved. If signs do not significantly improve in a week, there may be a need to perform further diagnostics.
Spectrum of care for $100-$500. Diagnostic testing can likely be limited to cytology if this is a first-time occurrence and as JC’s signs are not severe. Ideally, and if systemic antimicrobials are used in addition to the advised topical treatment, then C/S testing is performed at the start of treatment to ensure it is not a drug-resistant bacteria and inform us that, if systemic antibiotics are needed, we will have more confidence in their efficacy.
Total: $160-$500 Spectrum of care for over $500. Treatment can get to this price range if the infection is due to a drug-resistant bacteria, or there is an underlying skin or other condition.
Total: $600-$800 |
Michelle Evason, BSc, DVM, DACVIM (SAIM), MRCVS, serves as global director, Veterinary Clinical Education for Antech (MARS). Dr. Evason has worked in general practice, academia, specialty clinical practice, and in the animal health industry. She has published on numerous infectious diseases, antimicrobial stewardship, nutrition, spectrum of care, veterinary- and pet-owner education related topics.
Reference
- Loeffler A. Pyoderma. Weese JS, Evason M. Infectious Diseases of the Dog and Cat. CRC Press. July 2019. https://www.taylorfrancis.com/books/mono/10.1201/9780429186646/infectious-diseases-dog-cat-michelle-evason-scott-weese
- Hillier A, Lloyd DH, Weese JS, et al. 2014. Guidelines for the diagnosis and antimicrobial therapy of canine superficial bacterial folliculitis (Antimicrobial Guidelines Working Group of the International Society for Companion Animal Infectious Diseases)Vet Dermatol.25:163–175. https://pubmed.ncbi.nlm.nih.gov/24720433/
- Skin and ear infections. In: BSAVA/SAMSoc Guide to Responsible Use of Antibacterials: PROTECT ME. British Small Animal Veterinary Association; 2018.
- Stull JW, Shelby JA, et al. Barriers and next steps to providing a spectrum of effective health care to companion animals. J Am Vet Med Assoc. 2018. 253: 1386-1389. https://pubmed.ncbi.nlm.nih.gov/30451620/
- Fingland RB, Stone LR, et al. Preparing veterinary students for excellence in general practise: building confidence and competence by focusing on spectrum of care. J Am Vet Med Assoc. 2021. 259: 463-471. https://pubmed.ncbi.nlm.nih.gov/34388008/
- Launching an evidence-based veterinary medicine manifesto to drive better practise. Vet Rec. 2020: Sep;187 (5): 174-177. https://www.nottingham.ac.uk/cevm/about-the-cevm/evidence-based-veterinary-medicine-(evm).aspx
- Evidence-based veterinary toolkit, RCVS. https://knowledge.rcvs.org.uk/evidence-based-veterinary-medicine/ebvm-toolkit/. Accessed August 2021.
- Santoro D. Topical therapy for canine pyoderma: What is new? J Am Vet Med Assoc. 2023. 261: 140-148. https://pubmed.ncbi.nlm.nih.gov/36921021/