Pain management in dogs and cats is a critical component of veterinary care, encompassing various strategies and pharmaceutical options. As a veterinarian, it is essential to stay current on the latest advancements in pain management to ensure the well-being and comfort of our patients. This article provides a comprehensive overview of pharmaceutical pain management in dogs and cats, delving into the various pain assessment techniques, categories of pain medications, and the most recent scientific research in the field. It is aimed at equipping veterinarians with the knowledge and resources to make informed decisions about the pain management of their canine and feline patients.
Assessment
Pain is a complex sensory experience that can manifest differently in dogs and cats. Veterinarians must have a comprehensive understanding of how pain is expressed in these animals, allowing for effective assessment and treatment. Pain in dogs and cats can result from various sources, including injury, surgery, arthritis, dental disease, and chronic conditions. Pain can be categorized into two primary types: acute and chronic.
Acute pain is sudden and typically short-lived, resulting from injuries, surgeries, or acute medical conditions. It is usually easier to recognize because the signs are more pronounced and often include vocalization, agitation, restlessness, and/or changes in vital signs (i.e. increased heart rate or respiration rate).
Chronic pain persists over an extended period, typically greater than three months, often resulting from conditions, such as osteoarthritis, cancer, or intervertebral disc disease, among others. Detecting chronic pain can be challenging, as it may present with subtle signs, such as reduced activity, changes in posture, or altered behavior.
Accurate pain assessment is the foundation of effective pain management. Understanding how to evaluate and quantify pain in dogs and cats is important for individualizing treatment plans for patients. Multiple validated tools exist for veterinarians to aid in identifying pain, including:
- Pain scales. Various pain scales have been developed for dogs and cats. These tools provide quantitative measurements of pain intensity and can help veterinarians and pet owners gauge the intensity of pain and track its progression. Different tools can be used to aid in different situations, such as the Feline Grimace Scale,1 which is a validated scale for use by veterinarians in cases of acute pain in cats; or the Feline Musculoskeletal Pain Index,2 to be used primarily by owners in chronic pain and osteoarthritis situations,Validated tools for assessing pain in canine patients include the Glasgow Short Form scale3 for acute pain, and the Canine Brief Pain Index4 for chronic pain and osteoarthritis.
- Observational and behavioral changes. Observing and assessing changes in the animal’s behavior, posture, and mobility can provide valuable insights into the presence and intensity of pain. Subtle signs, such as licking, decreased appetite, and reluctance to move, or guarding specific body parts, can indicate pain. Pet owners may be especially helpful in identifying changes in pet behavior at home and may be able to video their pet’s mobility in a comfortable environment.
- Clinician assessment of pain. Veterinarians can assess for pain through observation of both the patient’s mobility and posture at rest. Patients may offload pain to unaffected limbs while walking or trotting, leading to gait abnormalities. At rest, abnormal limb positioning can indicate pain. Palpation is the most clinically used tool to evaluate for pain, and subtle signs, such as a change in respiratory rate or vocalization, can help identify if the patient is experiencing pain during palpation.5

Using the Feline Grimace Scale can help to identify pain in cats by looking at ear
position, orbital tightening, muzzle tension, whisker position, and head position.The Feline Grimace Scale
For more details and example photos, check out this article from the VPN Plus+ archives: “Benefits of using the Feline Grimace Scale“.
Not a member? Sign up today!
Management
Once pain is recognized and assessed, veterinarians have several options for managing pain in dogs and cats. These can include pharmacological and non-pharmacological approaches. Pharmacological pain management involves a variety of medications with different mechanisms of action and potential side effects. The choice of medication depends on the type and severity of pain, the individual patient’s condition, and the veterinarian’s assessment.
Common classes of pain medications for dogs and cats include:
- Non-steroidal anti-inflammatory drugs (NSAIDs). NSAIDs, such as carprofen and meloxicam, are commonly used for both acute and chronic pain relief in dogs and cats. They work by inhibiting cyclooxygenase enzymes, which reduces inflammation and pain associated with conditions such as osteoarthritis.
o Robenacoxib is a newer drug in this class licensed for use in both dogs and cats.6,7
o Grapiprant is also a newer medication that is available to manage chronic pain and works by blocking prostaglandin receptors.8
- Opioids, such as buprenorphine, are effective for managing moderate to severe pain. They work by binding to specific receptors in the brain and spinal cord to modulate pain perception. They are particularly useful post-surgery or for pain caused by injuries.
o Of note is a 24-hour subcutaneous injection labeled for use in cats, which can help with pain relief after discharge from the hospital due to its longer duration of action.9
o The use of oral tramadol in postoperative canine patients is not considered effective.5
o The long-term use of opioids for chronic pain control is generally not recommended.
- Gabapentin. This medication is often used for neuropathic pain, as seen in some chronic conditions. It works by down-regulating calcium channels, though the mechanism of action in pain regulation is not fully understood and the efficacy has not been scientifically proven.9
- Anti-nerve growth factor (NGF) monoclonal antibodies (mAb). A new development in the pain management toolbox is anti-NGF mAb. NGF plays an important role in nociception and anti-NGF antibodies have been shown to decrease hyperalgesia and pain behaviors in animals. Products have been approved for use in both dogs and cats to treat osteoarthritis-related pain.10,11
- Tricyclic antidepressants (TCAs), such as amitriptyline, may be used for chronic pain management, particularly when neuropathic pain is involved. They alter neurotransmitter levels in the central nervous system to reduce pain perception.9
- Ketamine/amantadine’s mechanism of action for pain control in dogs and cats involves N-methyl-D-aspartate (NMDA) receptor antagonism. By blocking these receptors in the central nervous system, ketamine disrupts the transmission of pain signals, leading to effective pain relief. Ketamine not only reduces pain perception but also helps maintain cardiovascular stability, making it a versatile and important component of anesthesia and pain control in veterinary practice.
o Amantadine has a similar mechanism of action as ketamine but can be dosed orally. Minimal data is available on the efficacy and suggested dosing of amantadine.5,9 - A2-adrenoceptor agonists, often used in combination with opioids, can be used perioperatively for analgesia and sedation. Their use should be carefully monitored and tailored to the individual patient needs due to the potential to cause severe cardiovascular and respiratory side effects. Examples of drugs in this class include dexmedetomidine and xylazine.9
- Local anesthetics. These should be employed during surgery or for localized pain management and include nerve blocks and injections. Lidocaine and bupivacaine have historically been the most commonly used medications in this category. A new long-acting bupivacaine formulation that is liposome-encapsulated can provide analgesia for up to three days post-operatively.5,9
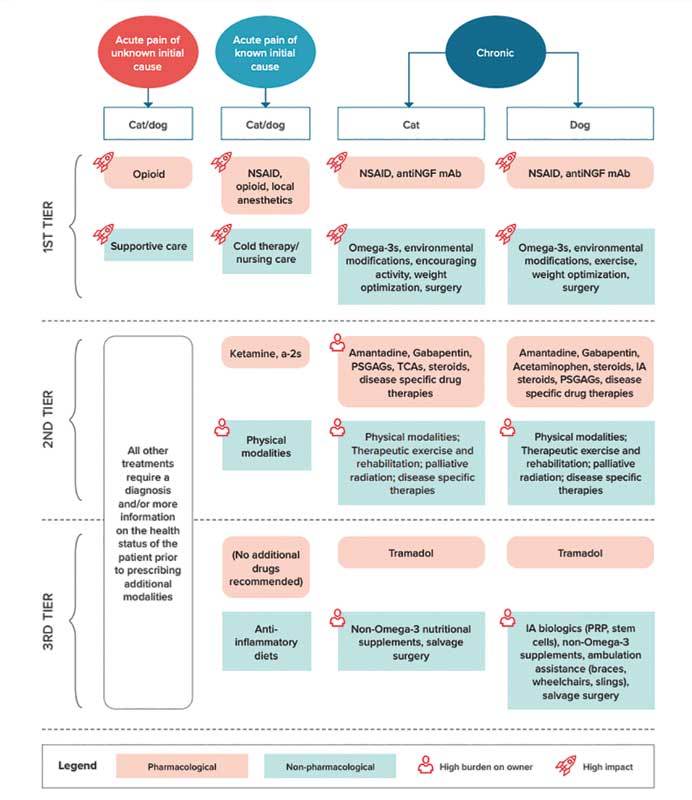
- The 2022 AAHA Pain Management Guidelines5 provides a decision tree (Figure 1) to aid in prioritizing the use of the most efficacious therapeutic modalities for both acute and chronic pain. Clinicians can employ strategies in multiple tiers at the same time.
Effectiveness and considerations
The effectiveness of pain medications in dogs and cats varies depending on the type and severity of pain in the individual patient. Factors to consider include:
- Pain type. Matching the right medication to the type of pain is essential. For example, NSAIDs are more effective for inflammatory pain, while opioids are better suited for severe, acute pain.
- Patient variation. Each animal may respond differently to medications. Some patients may experience more pain relief from one particular drug than another.
- Side effects. All medications have potential side effects, and some animals may be more prone to developing side effects. For instance, NSAIDs can sometimes cause gastrointestinal side effects, while opioids may lead to sedation and constipation.
- Underlying health conditions. The presence of underlying medical conditions can impact the choice of pain medication. Some medications are contraindicated in certain situations, making careful assessment by the
veterinarian crucial. - Long-term management. For chronic pain conditions, a long-term management plan is often necessary. This may involve a combination of medications, physical therapy, and lifestyle modifications.
- Multimodal analgesia consists of combining different drugs and therapies to address pain from various angles, thus providing more comprehensive pain relief. This can include both pharmaceutical and non-pharmaceutical therapies.
Non-pharmaceutical therapies that can be considered in a multi-modal approach include weight optimization, exercise and physical therapy, environmental modification, acupuncture, and nutritional supplements. Though an in-depth discussion of non-pharmaceutical therapies is outside the scope of this article, they have been used in multi-modal pain management plans with varying efficacy.5
Pain management in dogs and cats is a multifaceted and important aspect of veterinary care. Recognizing, assessing, and treating pain is not only essential for the comfort and well-being of our patients, but also contributes to their overall recovery and quality of life. Staying informed about the latest research and advancements is essential for providing the highest standard of care to our canine and feline patients. It is incumbent upon veterinarians and pet owners to work together, considering the specific needs surrounding each individual case, to ensure that pain management is comprehensive and effective. As our understanding of pain management in animals continues to evolve, the future holds promise for improved pain relief strategies and better quality of life for our companion animals.
Katie Krebs, DVM, MBA, DABVP (Canine and Feline) is an assistant professor in Clinical Primary Care at the University of Pennsylvania’s Ryan Veterinary Hospital. Dr. Krebs graduated from the University of California (UC), Davis School of Veterinary Medicine, with an emphasis in small animal medicine. Krebs completed a small animal rotating internship at the Atlantic Veterinary College in Prince Edward Island, Canada before completing a residency in Canine/Feline practice, American Board of Veterinary Practitioners (ABVP), and MBA at Virginia Tech. Her research interests include pain management of osteoarthritis in cats, preventative care and business education, and implementing telehealth for improved client communication.
References
- Evangelista MC, Watanabe R, Leung VSY, et al. Facial expressions of pain in cats: the development and validation of a Feline Grimace Scale. Sci Rep 2019;9:19128.
- Enomoto M, Lascelles BDX, Robertson JB, et al. Refinement of the Feline Musculoskeletal Pain Index (FMPI) and development of the short-form FMPI [published online ahead of print May 18, 2021]. J Feline Med Surg. doi:10.1177/1098612X211011984.
- Testa B, Reid J, Scott ME, Murison PJ, Bell AM. The Short Form of the Glasgow Composite Measure Pain Scale in Post-operative Analgesia Studies in Dogs: A Scoping Review. Front Vet Sci. 2021 Sep 30;8:751949. doi: 10.3389/fvets.2021.751949.
- Brown DC, Boston RC, Coyne JC, et al. Ability of the canine brief pain inventory to detect response to treatment in dogs with osteoarthritis. J Am Vet Med Assoc 2008;233:1278–83.
- Gruen, Margaret E, et al. “2022 AAHA Pain Management Guidelines for Dogs and Cats.” AAHA, 2022, www.aaha.org/aaha-guidelines/2022-aaha-pain-management-guidelines-for-dogs-and-cats/home/.
- Heit MC, Stallons LJ, Seewald W, et al. Safety evaluation of the interchangeable use of robenacoxib in commercially-available tablets and solution for injection in cats. BMC Vet Res 2020;16:355.
- Friton G, Thompson CM, Karadzovska D, et al. Efficacy and safety of oral robenacoxib (tablet) for the treatment of pain associated with soft tissue surgery in client-owned dogs. BMC Vet Res 2017;13:197.
- Rausch-Derra L, Huebner M, Wofford J, et al. A prospective, randomized, masked, placebo-controlled multisite clinical study of grapiprant, an EP4 prostaglandin receptor antagonist (PRA), in dogs with osteoarthritis. J Vet Intern Med 2016;30:756–63.
- Epstein, M. E., Rodan, I., Griffenhagen, G., et al. (2015). “2015 AAHA/AAFP pain management guidelines for dogs and cats.” Journal of the American Animal Hospital Association, 51(2), 67-84.
- Lascelles BD, Knazovicky D, Case B, Freire M, Innes JF, Drew AC, Gearing DP. A canine-specific anti-nerve growth factor antibody alleviates pain and improves mobility and function in dogs with degenerative joint disease-associated pain. BMC Vet Res. 2015 Apr 30;11:101. doi: 10.1186/s12917-015-0413-x.
- Enomoto M, Mantyh PW, Murrell J, et al. Anti-nerve growth factor monoclonal antibodies for the control of pain in dogs and cats. Vet Rec 2019;184:23.