Figure 2 (right): A thick saliva-like fluid is removed from an intraoral drainage site behind tooth 110.
Photos courtesy John R. Lewis
One of my professors in veterinary school (David Sweet, VMD, DAVDC) taught us the three rules of surgery: 1) Eat when you can, 2) Sleep when you can, 3) Don’t mess with the pancreas.
Oral surgery’s equivalent of rule No. 3 might be this: Don’t mess with the salivary ducts. A five-year-old spayed female dachshund was recently presented to me eight days after having extractions performed by her primary care veterinarian. She had multiple teeth extracted, including a right maxillary first molar tooth (tooth 109). For the first few days, she recuperated nicely, but on day five postoperatively, her appetite waned, and she developed swelling around the right eye and right-sided exophthalmos. Anti-inflammatories and antibiotics were tried, but by postoperative day eight, she was no better and was referred to us.
On initial exam, right-sided periorbital swelling extended caudally into the temporal muscle area, dorsal to the zygomatic arch. The third eyelid was prominent, and the right eye was exophthalmic and did not retropulse as well as the left eye (Figure 1). The extraction sites, including the site of the extracted 109, appeared to be healing nicely. Absorbable sutures were present in the area of the parotid and zygomatic papillae due to the flap closure of the 109 site. Discomfort was noted upon slight opening of the mouth, and, therefore, we did not attempt to fully open the mouth while the patient was awake.
Surgery and post-op
The patient was placed under general anesthesia. Opening of the mouth showed a normal range of motion. The palatal mucosa caudal to the right maxillary molars was ventrally deviated, swollen, and slightly ulcerated. The ulceration appeared to be associated with self-trauma from the swollen mucosa getting trapped between the caudal maxillary molars and mandibular molars. Contrast-enhanced cone beam CT scan showed an area of decreased uptake suggestive of fluid in the swollen temporal region and in the area of the zygomatic salivary gland. Aspirate of the swollen temporal area behind the eye initially showed no fluid when using a 20-gauge needle, but re-aspiration with an 18-gauge needle showed a thick clear fluid suggestive of inspissated saliva.
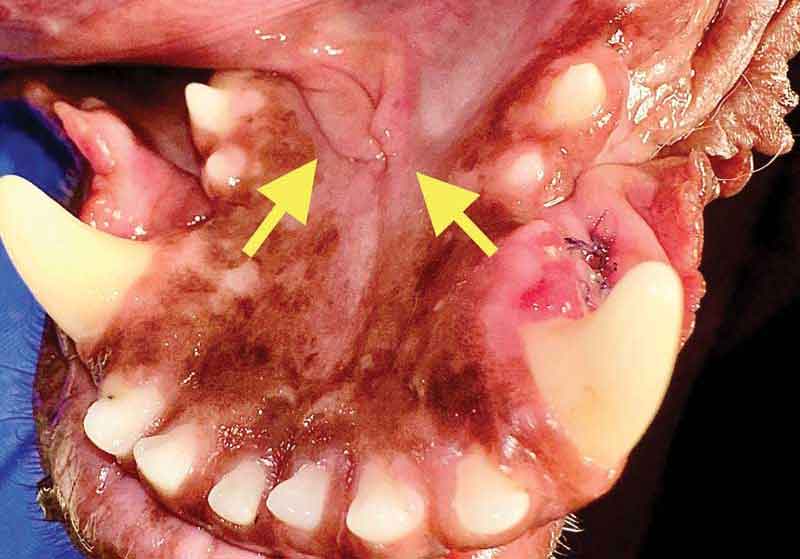
Closer inspection of the extraction site of tooth 109 showed a nicely healing mucoperiosteal flap. There were a few remaining sutures in the area of the zygomatic and parotid papillae, which were removed in case they were adversely affecting saliva transport. The area of swelling and ulceration behind tooth 110 was explored and opened with a pair of hemostats. A thick, clear fluid was suctioned out of the opening (Figure 2), suggestive of a zygomatic sialocele. The site was cultured, lavaged, and suctioned to remove as much of the saliva as possible. The area was left open to allow for drainage.
The patient was discharged with amoxicillin-clavulanate and carprofen. Owners were prepared for the possibility that if simple drainage of the area did not provide a resolution, removal of the zygomatic salivary gland would be necessary.
Reports from the owners over the subsequent days were positive, with an increase in appetite and a decrease in periorbital swelling and exophthalmos. However, approximately five days after the procedure, the swelling recurred and was worse than ever. A scab formed mediodorsal to the right eye, with some saliva-like drainage from this area.
The patient was placed under anesthesia and the zygomatic salivary gland was removed via a lateral approach after removal of a portion of the zygomatic arch. The salivary gland was submitted for histopathology, which showed mild inflammation, consistent with a sialocele or sialadenitis.

Recovery
Within days of removal of the zygomatic salivary gland, the swelling subsided, and the open area of the skin dorsal to the right eye began to heal. At the three-week postoperative recheck, exophthalmos resolved and the draining wound above the eye had closed (Figure 3).
This case reminds us of a rare complication of surgical extraction of the maxillary first molar tooth. I had seen a similar case years before in a Cavalier King Charles spaniel that had 109 extracted a week earlier. In the Cavalier’s case, abnormal accumulation of saliva responded to intraoral lancing and drainage of the area without removal of the gland. This complication has been previously described in the literature.1

Surgical tips
Recommendations to help minimize the chances of abnormal accumulation of saliva include identifying the salivary gland openings (papillae) prior to making incisions and carefully raising flaps. Place sutures in a way to avoid the papillae and the ducts that correspond to them. This is not merely a general practitioner issue: I recently received a call from a board-certified specialist who discussed a canine patient that underwent a bilateral rostral mandibulectomy and subsequently developed a ranula, even though the incision was just rostral to the mandibular and sublingual papillae.
The parotid and zygomatic salivary duct papillae can be seen in a raised crease of mucosa that sits dorsal to the maxillary first molar tooth. The parotid papilla is rostral and dorsal to the zygomatic papilla (Figure 4).
Similar caution should be taken when raising mucoperiosteal flaps or suturing near the papillae and ducts of the mandibular and sublingual salivary glands in the area of the rostral mandible and beneath the tongue. These papillae are referred to as caruncles and can be identified barely caudal to the caudal aspect of the mandibular symphysis (Figure 5). The salivary ducts course caudally from the caruncles and can be seen beneath the sublingual mucosa as a pale line, running in the furrow between the tongue and the mandible.
John Lewis, VMD, DAVDC, FF-OMFS practices and teaches at Veterinary Dentistry Specialists and Silo Academy Education Center, both located in Chadds Ford, Pa.
Reference
- Adams P, Halfacree ZJ, Lamb CR, Smith KC, Baines SJ. Zygomatic salivary mucocoele in a Lhasa apso following maxillary tooth extraction. Vet Rec. 2011;168(17):458. https://pubmed.ncbi.nlm.nih.gov/21493450